The integration of blockchain technology in healthcare promises to revolutionize the management of medical data, enhance security, and streamline operational processes. Despite its potential, widespread adoption remains limited, hindered by a complex interplay of technological, organizational, and external factors. This study develops an integrated theoretical model to identify and analyze these key drivers and barriers, […]
The integration of blockchain technology in healthcare promises to revolutionize the management of medical data, enhance security, and streamline operational processes. Despite its potential, widespread adoption remains limited, hindered by a complex interplay of technological, organizational, and external factors. This study develops an integrated theoretical model to identify and analyze these key drivers and barriers, […]
The integration of blockchain technology in healthcare promises to revolutionize the management of medical data, enhance security, and streamline operational processes. Despite its potential, widespread adoption remains limited, hindered by a complex interplay of technological, organizational, and external factors. This study develops an integrated theoretical model to identify and analyze these key drivers and barriers, providing valuable insights for healthcare providers, policymakers, and technology vendors seeking to accelerate blockchain implementation in hospitals. By grounding the research in well-established frameworks such as the Technology-Organization-Environment (TOE) model, the Fit Viability Model (FVM), and institutional theory, the study offers a comprehensive understanding of the multifaceted influences shaping adoption intentions. The empirical investigation, based on survey data from Malaysian hospitals, reveals critical determinants—including trust in technology, information transparency, organizational readiness, and external pressures—that significantly impact hospitals’ willingness to adopt blockchain-based health information systems (HIS). The findings also highlight the nuanced roles of hospital ownership types and regulatory environments, providing strategic guidance for fostering a more innovative and secure healthcare ecosystem. For further case illustrations, explore examples of AI applications in healthcare or how AI assists daily healthcare operations, which complement technological adoption insights. The study underscores that aligning technological attributes with organizational needs and external influences is vital for successful blockchain integration, paving the way for smarter, safer, and more efficient healthcare services.
Introduction
The healthcare industry is increasingly driven by digital transformation, aiming to improve patient outcomes, operational efficiency, and data security. Blockchain technology (BCT), with its decentralized, transparent, and tamper-proof features, has emerged as a promising solution to longstanding challenges such as data breaches, interoperability issues, and administrative inefficiencies. However, despite its potential, the actual adoption of blockchain in healthcare organizations remains modest. Numerous internal and external factors influence this hesitation, including trust in new technology, organizational capacity, regulatory pressures, and market competition. Understanding these factors comprehensively is crucial for designing effective strategies that promote blockchain integration. This research employs a hybrid theoretical approach, integrating the TOE framework, the Fit-Viability Model, and institutional theory, to systematically examine the determinants influencing hospitals’ intentions to adopt blockchain-based health information systems (HIS). The study focuses on Malaysian hospitals, providing context-specific insights that can inform policy and practice in emerging healthcare markets. The findings offer a pathway to harness blockchain’s full potential in advancing healthcare data security, interoperability, and efficiency.
Literature Review
Current State of Blockchain Adoption in Healthcare
Blockchain’s application in healthcare is gaining attention for its ability to enhance data security, enable interoperability, and automate workflows via smart contracts. Nonetheless, empirical studies exploring organizational-level adoption factors are limited. Most existing research centers on technical challenges or conceptual frameworks, with few examining the broader organizational, institutional, and environmental influences. For instance, studies from countries like India and South Korea reveal barriers such as regulatory uncertainty, high costs, and lack of expertise, which impede adoption efforts. Similarly, research in Canada and Thailand emphasizes concerns over data privacy, stakeholder trust, and regulatory compliance. These insights underscore the importance of understanding contextual factors that influence decision-making in healthcare organizations. A significant research gap exists in comprehensively analyzing how organizational readiness, external pressures, and technology attributes jointly affect blockchain adoption, especially in diverse healthcare settings such as public versus private hospitals.
Theoretical Foundations for Adoption Modeling
The TOE framework provides a holistic lens by considering technological, organizational, and environmental factors that influence innovation adoption. The Fit-Viability Model complements this by evaluating how well a technology aligns with organizational needs and whether it is feasible given available resources. Institutional theory adds depth by accounting for external pressures, such as regulatory mandates, mimetic behavior, and normative influences. Combining these models allows for a nuanced analysis that captures both internal capabilities and external stimuli shaping hospitals’ adoption intentions.
Research Model and Hypotheses
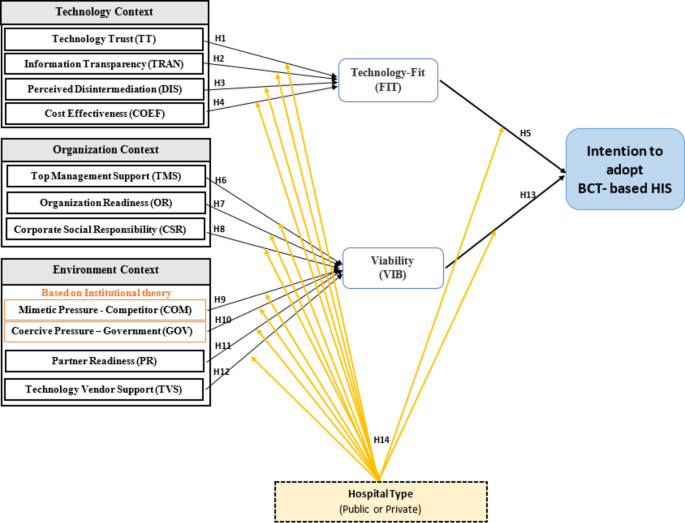
Drawing from the integrated frameworks, the proposed model includes technological factors (trust, transparency, disintermediation, cost-effectiveness), organizational factors (management support, organizational readiness, corporate social responsibility), external pressures (mimetic, coercive, partner, vendor support), and contextual moderators (hospital ownership type). These constructs influence the perceived fit and viability of blockchain HIS, which in turn affect the intention to adopt. The hypotheses posit that:
- Trust in blockchain significantly enhances perceived technology fit.
- Transparency of healthcare data positively influences fit.
- Perceived disintermediation improves the alignment with organizational processes.
- Cost-effectiveness significantly impacts fit.
- Good technology fit and perceived viability increase adoption intention.
- Organizational support and readiness bolster viability.
- External pressures such as government mandates and competitive mimicry influence viability.
- Support from partners and vendors enhances perceived viability.
- Hospital ownership type moderates these relationships.
Methodology
Data Collection and Sample
A structured survey instrument was developed, comprising 66 items measuring 14 constructs, adapted from validated sources. The questionnaire employed a five-point Likert scale and was pre-tested through expert reviews and a pilot study to ensure reliability and validity. The survey targeted senior managers and IT professionals in Malaysian hospitals, stratified by hospital ownership type, resulting in 199 usable responses out of 295 distributed questionnaires. Data collection was conducted online, leveraging official hospital contacts to reach a geographically dispersed population.
Data Analysis
Partial least squares structural equation modeling (PLS-SEM) was employed for hypothesis testing and model validation, given its suitability for exploratory research and complex models with smaller samples. Reliability and validity assessments confirmed the robustness of the measurement model, while path analysis tested the hypothesized relationships. Multi-group analysis evaluated the moderating effect of hospital type, and the model’s explanatory power was assessed through R², effect sizes, and predictive relevance measures.
Results and Discussion
Empirical findings support several key hypotheses: trust, transparency, disintermediation, and cost-effectiveness significantly enhance blockchain’s perceived fit within healthcare systems. Organizational support mechanisms, including top management backing, organizational readiness, and vendor support, positively influence perceived viability. External pressures such as government policies exert a negative impact on viability, indicating regulatory hurdles currently hinder adoption. Interestingly, hospital ownership type did not significantly moderate the relationships, suggesting that internal and external factors influence both public and private hospitals similarly in this context.
The model explains over 60% of the variance in adoption intention, emphasizing the importance of aligning technology attributes with organizational capacity and external environment. These insights suggest that fostering trust, ensuring organizational preparedness, and clarifying regulatory frameworks are critical steps toward accelerating blockchain adoption in healthcare.
Practical Implications
Healthcare practitioners and policymakers can leverage these findings to formulate targeted interventions. Building trust through transparent data management and demonstrating cost savings can motivate adoption. Strengthening organizational readiness via staff training and management support is crucial. Policymakers should streamline regulations and provide clear guidelines to mitigate negative external pressures. Technology vendors must offer comprehensive support, including customization and training, to facilitate implementation. Promoting collaboration among hospitals, regulators, and suppliers can create a conducive environment for blockchain integration.
Limitations and Future Research
This study’s scope is limited to Malaysian hospitals, and findings may differ in other healthcare systems with varying regulatory and cultural contexts. Longitudinal studies are needed to observe adoption dynamics over time. Incorporating patient and healthcare professional perspectives can deepen the understanding of acceptance factors. Future research should also explore privacy concerns inherent in blockchain applications, balancing transparency with data security requirements, such as compliance with regulations like HIPAA or medical data privacy guidelines. Expanding the model to include technological maturity levels and market readiness can further refine adoption strategies.
Conclusion
This study confirms that blockchain technology’s adoption in healthcare is influenced by a complex set of technological, organizational, and external factors. By integrating multiple theoretical perspectives, it provides a comprehensive framework for understanding and promoting blockchain implementation in hospitals. The findings indicate that building trust, ensuring organizational preparedness, and addressing external regulatory and competitive pressures are vital for advancing healthcare digitalization. Although hospital ownership does not significantly alter these relationships, targeted strategies that consider hospital-specific contexts remain essential. Ultimately, aligning technological attributes with organizational and environmental factors will be key to realizing blockchain’s transformative potential in healthcare, leading to more secure, efficient, and patient-centered services.